Tibialis Posterior Tendinopathy
Tibialis Posterior Pathologies
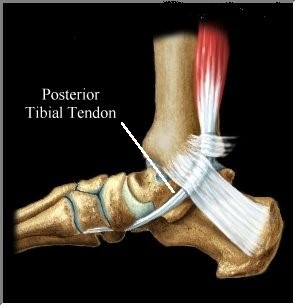 The tibialis posterior tendon is an imperative part of your heel and ankle as it starts deep within the calf and runs behind the medial malleolus (inner ankle bone) on the inner part of the heel. The tendon then inserts into multiple locations on the inside and bottom of the arch. In regular day-to-day activities, tremendous tension and stress is placed upon the tendon as it helps to maintain the arch of the foot, prevent excessive flattening (over pronation) and then contracts to help the foot ‘push off’. This tendon works even harder with running and high impact activities
The tibialis posterior tendon is an imperative part of your heel and ankle as it starts deep within the calf and runs behind the medial malleolus (inner ankle bone) on the inner part of the heel. The tendon then inserts into multiple locations on the inside and bottom of the arch. In regular day-to-day activities, tremendous tension and stress is placed upon the tendon as it helps to maintain the arch of the foot, prevent excessive flattening (over pronation) and then contracts to help the foot ‘push off’. This tendon works even harder with running and high impact activities
How do I know if I have Tibialis Posterior Tendinopathy?
Tibialis posterior tendinopathy can often be mistaken as a chronic rolled ankle as symptoms include pain and swelling along the inside of the ankle and arch following the course of the tendon. Therefore, it is important to go to a foot expert for proper diagnosis. In many cases the pain may be present when walking, running or during extended periods of standing and commonly there will be pain and weakness to rise onto your toes. There can also be flattening/collapse of the arch, outward pointing of the foot and an inward rolling of the ankle
What causes Tibialis Posterior Tendinopathy?
Tibialis posterior tendinopathy is the term given to any inflammation or degeneration to the posterior tibial tendon. Due to the large amount of force that goes through this tendon, the most common cause of tibialis posterior tendinopathy is overuse or sudden injury. Overuse leads to inflammation of the tendon and tendon sheath, which over time can often lead to degeneration (tendinosis) of the tendon. More causes consist of:
- A sudden increase in activity or high impact exercise including running
 , walking, hiking or climbing stairs which proves to be too much for the tendon to cope with.
, walking, hiking or climbing stairs which proves to be too much for the tendon to cope with. - An ankle sprain or trauma to the area with inflames the area and inhibits the tendon to function properly
- Repetitive strain due to poor biomechanics – (pronated or flat feet).
- Weakness through calf complex and the tibialis posterior muscle which overloads the tendon.
- Improper footwear with poor stability and support.
Can Tibialis Posterior Tendinopathy progress? How serious can it get?
If tibialis posterior tendinopathy continues to flare up, becomes chronic and it is not appropriately treated, discomfort will increase and it may progress to tibialis posterior tendinosis (degeneration) and then tibialis posterior dysfunction. The progression of these conditions generally develops in the following order:
- Tibialis Posterior flare up and tendinopathy – when the pain in the tendon first occurs following an injury, tear or overuse.
- Tibialis Posterior tendinosis – when the tendon pain has been present for some time (over 3 months) and the tendon becomes painfully degenerated. At this stage, it is not just inflamed but rather weak, slightly lengthened and consistently painful.
- Tibialis Posterior dysfunction – when the damage is so severe that there is noted lengthening and degeneration of the tendon accompanied by strength deficit and inability to walk without pain or rise onto toes.
Tibialis Posterior Dysfunction
Tibialis Posterior tendon dysfunction is also known as adult acquired flatfoot where the tendon can no longer support the arch, which results in the flattening/collapse of the foot. Often people will notice that their ‘arches have dropped’. Although this condition typically only occurs in one foot, it can develop in both feet. As this dysfunction becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot to the heel and below the ankle due to compensations. During this time, the foot can also become rigid as the tendon has deteriorated considerably and arthritis can develop in the foot due to joint overload.
can no longer support the arch, which results in the flattening/collapse of the foot. Often people will notice that their ‘arches have dropped’. Although this condition typically only occurs in one foot, it can develop in both feet. As this dysfunction becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot to the heel and below the ankle due to compensations. During this time, the foot can also become rigid as the tendon has deteriorated considerably and arthritis can develop in the foot due to joint overload.
What treatments are used to manage Tibialis Posterior Tendinopathy?
Treatment for this particular heel pain condition depends on the severity of the symptoms, the time frame of the pain and the function of the tendon. Treatment must take into account the cause of the problem and whether or not the tendon is inflamed &/or degenerated, how much strength loss has occurred (if any) and if there it has progressed to tibialis posterior tendon dysfunction. Often if identified early and the tendon is preserved the treatment can often be quite successful with conservative options including ice, activity reduction, appropriate footwear, strapping and a tendon strengthening program.
Often as heel pain experts we see this condition when it is more advanced and the tendon has started to degenerate which requires a more in-depth treatment plan. This can include the conservative options combined with things such as corrective orthotics to reduce tendon stresses, promote tendon healing and allow return to normal activities. If symptoms are still present then injection therapy may be warranted to reduce pain levels, a specific ankle and foot combination bracing or even an immobilisation boot to allow the tendon to completely heal.
In the most severe cases surgical repair may be required to restore lost function but very infrequently and as a last resort only.
Due to the progressive state of tibialis posterior tendon pain around your heel it is best to see your heel pain expert for early intervention as one consultation could put your mind at ease and avoid a lot of unnecessary pain and restrictions to your lifestyle!
